Providers are making progress on reducing healthcare-associated infections
 Healthcare in the U.S. is safer now than it was 10 years ago, according to recent data compiled by the Centers for Disease Control and Prevention.
Healthcare in the U.S. is safer now than it was 10 years ago, according to recent data compiled by the Centers for Disease Control and Prevention.
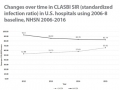
The incidence of central-line-associated bloodstream infections (CLABSIs) dropped significantly between 2008 and 2016, while catheter-associated urinary tract infections (CAUTIs) have dropped as well, most markedly in non-ICU locations. And while surgical site infections are on the decline, progress may be slowing following some procedures.
The data was published recently by CDC in “Healthcare-associated Infections in the United States, 2006-2016: A Story of Progress.”
“Infection preventionists nationwide are seeing the positive effects of HAI [healthcare-associated infection] reduction efforts initiated in the early 2000s,” says Marie H. Wilson, BSN, BS, RN, CIC, infection preventionist at Methodist Dallas Medical Center.
“CDC’s National Healthcare Safety Network – NHSN – established a new baseline comparison for HAI Standardized Infection Ratios – SIRs – with data aggregated from 2015,” says Wilson, who is a member of the communications committee of the Association for Professionals in Infection Control and Epidemiology. “As a result of this ‘rebaseline,’ it’s now harder to achieve lower SIRs – a sign that fewer infections are predicted. This is a direct result of HAI prevention initiatives seen nationwide, including safer and reduced use of indwelling devices and antimicrobial stewardship programs.”
“The CDC’s report confirms we’re driving the needle of change toward zero HAIs.”
National action plan
In 2009, the U.S. Department of Health and Human Services published the “National Action Plan to Prevent Health Care-Associated Infections: Road Map to Elimination,” which set five-year goals for HAI prevention.
CDC publishes yearly reports to help each state identify its progress and target areas that need assistance. The data used in these reports comes from two surveillance systems: the National Healthcare Safety Network (NHSN) and the Emerging Infections Program Healthcare-Associated Infections Community-Interface (EIP HAIC).
In addition, CDC and other federal agencies, such as Centers for Medicare and Medicaid Services, the Agency for Healthcare Research and Quality and the Office of the Assistant Secretary for Health, work together to develop tools, recommendations, and programs that offer infection prevention strategies.
In its most recent report, CDC examines the nation’s progress preventing five of the most common infections:
- Central-line-associated bloodstream infections (CLABSI).
- Catheter-associated urinary tract infections (CAUTI).
- Select surgical site infections (SSI).
- Hospital-onset Clostridium difficile infections (CDI).
- Hospital-onset methicillin-resistant Staphylococcus aureus (MRSA) bacteremia (bloodstream infections).
Central Line-Associated Bloodstream Infection (CLABSI)
Nationally, CLABSIs dropped roughly 50 percent between 2008 and 2016. The data also shows a reduction in the use of central lines. “Carefully determining the necessity of central lines before insertion is a CLABSI prevention strategy,” points out CDC.
The magnitude of SIR (standardized infection ratio) declines from 2012-2014 leveled off, a trend that was more pronounced on wards, to which the majority of CLABSIs were attributed in 2015, says CDC. And recent unpublished data suggests that, at least among adult intensive care unit (ICU) patients, declines in CLABSIs caused byStaphylococcus and Enterococcus spp. have outpaced declines in infections caused by gram negative and fungal pathogens.
Catheter-associated Urinary Tract Infection (CAUTI)
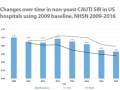
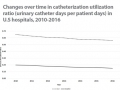
After an early lack of progress, CAUTIs have been steadily declining over the past few years. The gains have been most marked in non-ICU locations, but recent years have seen progress in ICUs as well. Data also indicates a reduction in urinary catheter usage – a key prevention strategy for CAUTI.
Although CAUTIs that include those caused by yeast declined on wards from 2012 through 2014, they failed to decline in ICUs. However, using the more clinically relevant CAUTI definition, which no longer includes yeast, and applying this retrospectively as well as in the new baseline, there were year-to-year declines in CAUTIs in both ICUs and wards from 2012 through 2016.
The removal of yeast from CAUTI reports from 2009 through 2014 shows that reductions in wards – to which a slight majority of CAUTIs were attributed in 2015 – were more pronounced. However, there were also declines in the ICU SIR, resulting in successive yearly relative declines of 6-8 percent in the CAUTI SIR from 2012 through 2014.
Surgical site Infections
Overall, the incidence of surgical site infections has dropped since 2010. That said, progress may be slowing following some procedures.
Clostridium difficile Infection (CDI)
Crude rates of healthcare-associated CDI are decreasing, reflecting declines in nursing home-onset infections along with some declines in hospital-onset CDI, says CDC. An assessment of CDI events reported to NHSN demonstrates that nearly 70 percent of reported events had their onset in the community in 2015.
Methicillin-resistant Staphylococcus aureus Bacteremia (MRSA Bacteremia)
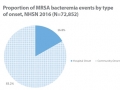
There has been major progress since 2005 in preventing MRSA bacteremia due to declines in hospital-onset and community-onset, healthcare-associated bacteremia. Much of the progress reflects improvements in preventing insertion-related CLABSIs.
More than 80 percent of reported events in 2015 had their onset in the community. There has been little or no decline in community-associated MRSA bacteremia, suggesting a need for a comprehensive, multidisciplinary, community-based public health approach to prevention of invasive infections caused by this common skin organism, says CDC.
“The fact that the community burden of MRSA bloodstream infections isn’t worsening is a testament to the work infection preventionists are doing in collaboration with physicians and pharmacists on antimicrobial stewardship programs,” says Wilson. “CDC’s National Action Plan for Combating Antibiotic-Resistant Bacteria (2015) outlines several goals and objectives many groups and individuals can employ to reduce the impact of multidrug-resistant organisms across the board.”
Editors note: “Healthcare-associated Infections in the United States, 2006-2016: A Story of Progress” may be accessed at https://www.cdc.gov/hai/surveillance/data-reports/data-summary-assessing-progress.html