Morale among physicians may not be great, but it’s getting better
A changing of the guard is taking place among physicians. Physicians themselves, staff, patients and distributor sales reps will more than likely feel the impact.
“America’s physician workforce is undergoing significant changes,” Walker Ray, M.D., vice president of The Physicians Foundation and chair of its research committee, was quoted as saying, following the release of “The Physicians Foundation’s 2014 Survey of America’s Physicians,” conducted by Merritt Hawkins. “Physicians are younger, more are working in employed practice settings and more are leaving private practice.”
This “new guard” of physicians report having less capacity to take on additional patients, a trend that could have implications for patient access to care, he said. But they are also somewhat optimistic about the future of medicine.
The survey, conducted online from March 2014 through June 2014, is based on responses from 20,088 physicians across the United States.
Changing attitudes
Relative to the national surveys The Physicians Foundation conducted in 2012 and 2008, doctors are more positive in their outlook as their ranks change demographically and as their status rapidly shifts from that of independent practice owner to employee, according to Merritt Hawkins.
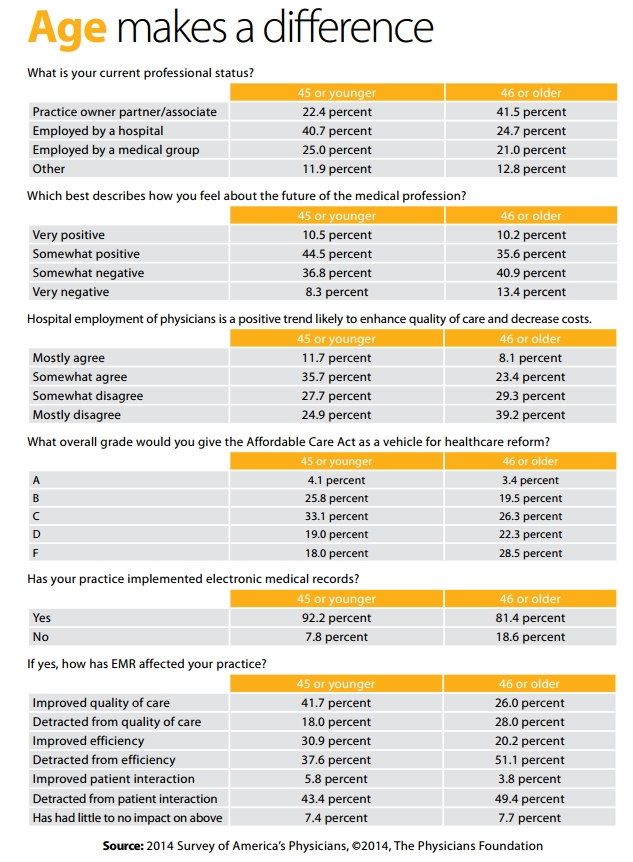
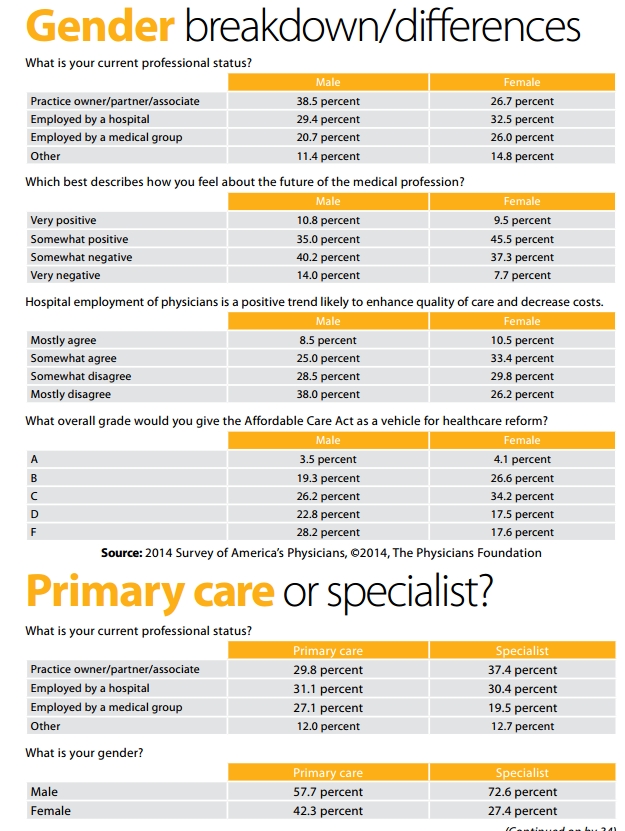
Respondents to the 2014 survey are younger, and more likely to work in employed settings (e.g., hospital systems), compared to those in earlier surveys. Percentage-wise, more are females, and more work in primary care. In 2014, the average age of the respondents is 50, vs. an average age of 54 in 2012. In 2014, 33 percent of the survey respondents are female, vs. 26 percent in 2012. Survey respondents mirror the composition of the current U.S. physician workforce, according to Merritt Hawkins.
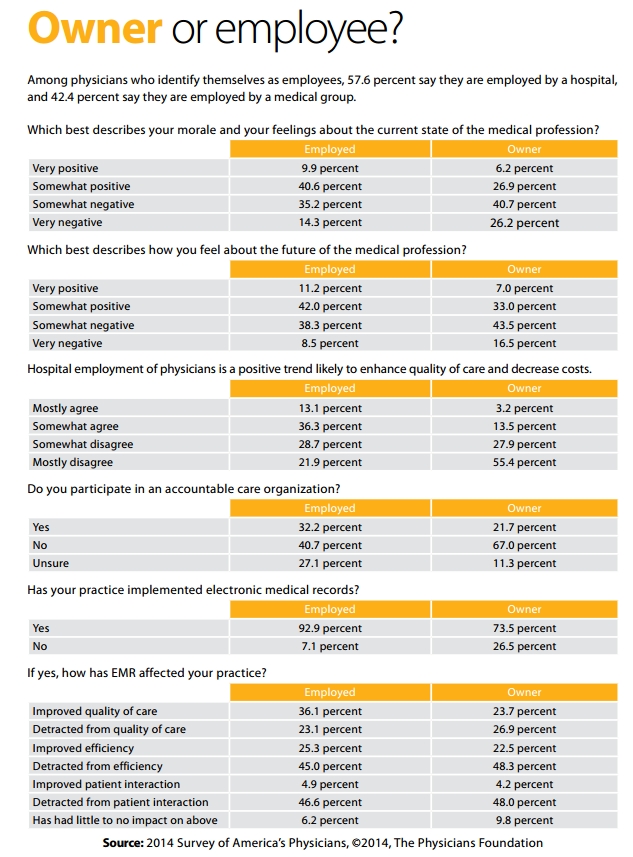
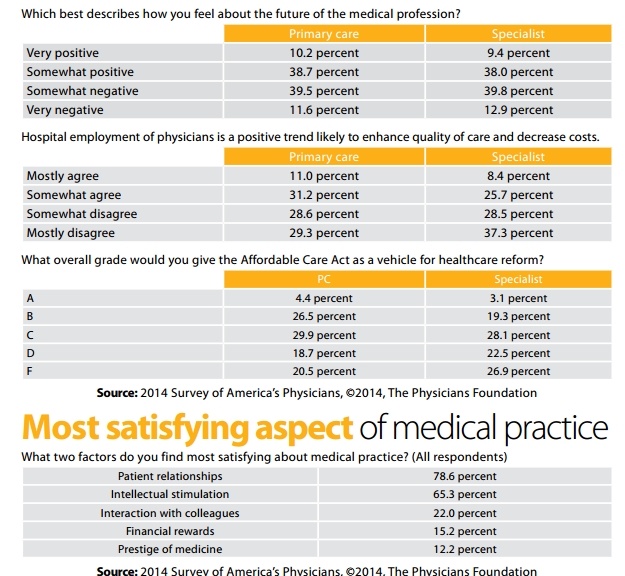
Physicians are not uniform in their perspectives. Younger physicians, female physicians, employed physicians and primary care physicians are more positive about the current medical practice environment than are older physicians, male physicians, medical specialists and practice owners. Even so, the majority of almost all groups suffer from low morale and express doubts about the direction of the healthcare system. In addition, more than two-thirds of employed physicians (68 percent) expressed concerns relative to clinical autonomy and their ability to make the best decisions for their patients.
Practice ownership
- Only 35 percent of physicians describe themselves as independent practice owners, down from 49 percent in 2012 and 62 percent in 2008.
- Fifty-three percent of physicians describe themselves as hospital or medical group employees, up from 44 percent in 2012 and 38 percent in 2008.
- Only 17 percent of physicians indicate they are in solo practice, down from 25 percent in 2012.
Capacity
- Eighty-one percent of physicians describe themselves as either overextended or at full capacity, up from 75 percent in 2012 and 76 percent in 2008. Only 19 percent say they have time to see more patients.
- Forty-four percent of physicians plan to take one or more steps that would reduce patient access to their services, such as seeing fewer patients, retiring, working part-time, closing their practice to new patients, or seeking a non-clinical job, leading to the potential loss of tens of thousands of full-time-equivalents (FTEs).
- Twenty-four percent of physicians either do not see Medicare patients or limit the number of Medicare patients they see.
- Thirty-eight percent of physicians either do not see Medicaid patients or limit the number of Medicaid patients they see.
- Nevertheless, on average, more than 49 percent of the patients physicians do see are enrolled in Medicare or Medicaid.
- Seventy-two percent of physicians believe there is a physician shortage, that more physicians should be trained, and that the cap on funding for physician graduate medical education should be lifted.
Morale
- Only 29 percent of responding physicians would not choose medicine if they had their careers to do over, a decrease from 35 percent in 2012.
- Forty-four percent of physicians describe their morale and feelings about the current state of the medical profession as positive, an increase from 32 percent in 2012.
- Fifty percent of physicians would recommend medicine as a career to their children or other young people, an increase from 42 percent in 2012 and 40 percent in 2008.
- Sixty-nine percent of physicians believe that their clinical autonomy is sometimes or often limited and their decisions compromised.
- Physicians work an average of 53 hours a week, virtually the identical number of hours they reported working in 2012, but down from 57 hours in 2008.
- Fifty percent of physicians indicate their belief that implementation of ICD-10 will cause severe administrative problems in their practices.
- Physicians spend 20 percent of their time on non-clinical paperwork.
- Thirty-nine percent of physicians indicate they will accelerate their retirement plans due to changes in the healthcare system.
Healthcare reform
- Forty-six percent of physicians give the Affordable Care Act a D or F grade, while 25 percent give it an A or B.
- Eighty-five percent of physicians have adopted electronic medical records (EMR), up from 69 percent in 2012. However, 46 percent indicate EMR implementation has detracted from their efficiency, while only 24 percent say it has improved their efficiency.
- Seven percent of physicians now practice some form of direct pay/concierge medicine, while 13 percent indicate they plan to transition in whole or in part to this type of practice. Seventeen percent of physicians 45 or younger indicate they will transition to direct pay/concierge practice.
- Thirty-three percent of physicians currently participate in insurance products offered through their state/federal marketplace exchanges, while 28 percent say they have no plans to.
- Twenty-six percent of physicians now participate in an accountable care organization, though only 13 percent believe ACOs will enhance quality and decrease costs.
Physician morale
Although the physicians responding to the 2014 survey are more positive in their perspectives than physicians who responded to the 2012 survey, these positive feelings are relative and not absolute, according to Merritt Hawkins. The 2014 survey shows what may be an incipient change in physician attitudes for the better, many physicians today continue to express a low level of morale and significant misgivings about the state of their profession and the healthcare system.
Responses to the morale question show that the “new guard” of medicine — including younger physicians, female physicians, employed physicians and primary care physicians — expressed considerably higher levels of professional morale than did “old guard” physicians, including those over age 45, male physicians, practice owners and specialists.
This gap is most apparent among employed physicians, 50.6 percent of whom described their morale as very or somewhat positive, compared to only 33.1 percent of practice owners. Similarly, 50.2 percent of primary care physicians described their morale as very or somewhat positive compared to only 40.7 percent of specialists. The majority of physicians 45 or younger (54.3 percent) described their morale as very or somewhat positive, compared to only 38.9 percent of physicians 46 or older.
The relatively positive feelings expressed by younger physicians may be in part a result of the fact that most doctors under the age of 45 entered the profession when changes to physician practice structures and reimbursement already were underway, according to the researchers. Since many have always been employed and have no basis for comparing the employed practice model to the independent model.
Autonomy in clinical decision-making
Fewer than one-third of physicians say they are free to make the best decisions for their patients, while 69 percent say their medical decisions are sometimes or often compromised. Responses to this question vary only marginally among various physician types, notes the researchers.
What may be most notable about responses to the question about clinical autonomy is that employed physicians indicated their clinical autonomy is slightly less limited than practice owners, by a margin of 68.2 percent to 70.6 percent. This contradicts the widely held perception that physicians sacrifice their clinical autonomy to become employees in exchange for security, while practice owners sacrifice security to preserve clinical autonomy, Merritt Hawkins researchers note. In fact, the survey suggests that many employed physicians and practice owners feel their clinical autonomy is limited, in close to equal numbers. This may in part be a result of more robust clinical analytics than existed in the past, which, by outlining treatment protocols for various medical conditions, have taken some of the subjectivity out of medicine.
Physician supply and patient access
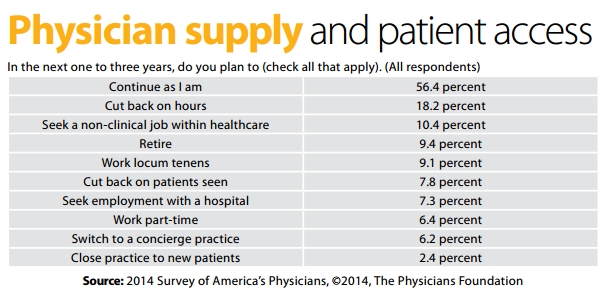
The majority of physicians (56.4 percent) indicated they will continue practicing as they are. Over 40 percent, however, said they will take one or more steps likely to reduce patient access to their services. Over 9 percent of physicians indicated they will retire in the next one to three years. Should they do so, approximately 72,000 physicians would be removed from the workforce, note the researchers. Over 10 percent said they will seek non-clinical jobs within healthcare, an occurrence that would remove an additional 80,000 physicians from the workforce. Over 18 percent said they will cut back on hours, while 7.8 percent said they will cut back on the number of patients they see. An additional 29.2 percent said they will adopt a style of practice (concierge, locum tenens, part-time, or hospital employed) likely to reduce their patient load.
That the physician workforce can ill-afford the loss is underscored by physicians themselves, note the researchers. When asked to describe their practices, over 81 percent of physicians said that they are either at full capacity or are overextended and overworked, up from 75.5 percent in 2012. Only 19 percent indicated they have the time to see more patients and assume more duties, down from 24.5 percent in 2012.
Whether or not the growing number of Medicare and Medicaid enrollees will have reasonable access to a physician is an open question, according to Merritt Hawkins. About one quarter of physicians responding to the survey now no longer see Medicare patients or limit the number they see, while 38.1 percent no longer see Medicaid patients or limit the number they see. By contrast, in 2012, only 8.6 percent of physicians said they had closed their practices to Medicare patients while 26.7 percent said they had closed their practices to Medicaid patients.
Given the potential shortage of physicians, it would be advantageous if doctors could devote a minimal amount of time to tasks not directly related to patient care. However, the survey indicates that physicians spend 10.58 hours a week on non-clinical paperwork duties, or 20 percent of their total work hours. However, in a positive development, physician work hours spent on non-clinical duties decreased in 2014 relative to 2008, when physicians reported spending 15.19 hours, or 26 percent of their time, on non-clinical duties; and also decreased relative to 2012, when physicians reported spending 12.01 hours, or 22.6 percent of their time, on non-clinical duties. These numbers suggest administrative efficiency gains have been achieved, possibly through the increased or more strategic use of information technology, including EMR, through enhanced management techniques, or for other reasons, according to Merritt Hawkins.
Notable here is that employed physicians report working more hours per week on non-clinical duties than do practice owners. Employed physicians report spending 10.63 hours per week on non-clinical paperwork, while owners report spending 9.79 hours. One of the presumed benefits of physician employment is that it frees doctors from the non-clinical duties of running a practice with which practice owners must contend, and therefore allows them to spend more time with patients. Both the 2014 and the 2012 surveys suggest this is not the case.
Editor’s note: To receive a copy of the 2014 Survey of America’s Physicians, go to www.physiciansfoundation.org