By Laurie Morgan
partner and consultant, Capko & Morgan
Capko & Morgan has recently teamed up with demand-generation firm MedData Group to survey doctors on key practice management issues. This summer’s “MedData Point” study was on revenue cycle management, AKA medical billing. It’s a subject that’s central to our practice management consulting work. (Getting paid is always on the minds of our clients.) But despite our regular access to in-person feedback from physicians about billing, the survey still held some surprises. Some of these evolving concerns may represent both a problem and an opportunity for your business.
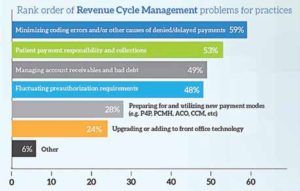
One notable surprise was the resurgence of concerns about health plan reimbursements. For the past few years, our clients have been most vocal about patient collections, thanks to increasing deductibles. As the survey graphic below shows, collecting from patients is still a very pressing concern. But even more physicians expressed concern about denied and delayed claims. Do your clients know how to properly document and code for your products, to avoid denials and extra steps to appeal them?
 (Source: MedData Group. Complete results and infographic available at: https://www.meddatagroup.com/news/meddata-point-research/)
(Source: MedData Group. Complete results and infographic available at: https://www.meddatagroup.com/news/meddata-point-research/)
A related response, fluctuating preauthorization requirements, was also a bit of a surprise. Not because preauthorizations are a new frustration; we’ve been hearing this complaint for years. But the fact that nearly half of respondents, drawn from all specialties, cite this issue as a pressing concern is interesting. The burden of preauthorization appears to be rising again, after seeming to stabilize for a few years. Cost-control pressures of healthcare reform may be driving payers, including Medicare, to require more prior authorizations for devices; with many drugs hitting or approaching patent cliffs, payers are also focusing on substituting generics. In specialties like rheumatology, increasing use of costly biologics may also be contributing to the trend.
Lending a hand
Vendors and reps that help practices navigate this tedious process stand out in a very positive way. And there are easy ways to make a difference. For example, could you publish a list of popular health plans that require preauthorization for your product or service? (We know of one regional diagnostic lab that has a handy chart on their website for this purpose.)
Technology platforms that can help are also emerging. Will your product(s) be available on online services that allow prior authorizations to be done more efficiently? Equally important, do your clients know about this capability? In our experience, technology utilization by practices usually has much room for improvement.
Even the practice management and EMR systems practices already own are often used at only a fraction of their potential. That’s why another standout survey result – the mere 24 percent of respondents who said upgrading front office technology is a pressing concern – was, unfortunately, not a surprise.
Achieving awareness and understanding of technology that can solve practice management problems is no small feat. Even as neutral consultants, we often find it hard to make the message stick. If technology is what you’re selling, and you’re facing an uphill mindshare battle, know that it’s not just you. But also know that if your help eventually enables a practice to simplify a workflow or billing hassle, you will break away from the field by becoming a trusted resource.